 |



|
|
| About Us | Community Services | Public Education | Annual Scientific Meeting | Members' Area |
Public Education >
| HKOS in the News |
| 眼睛解碼 |
| The Roles of Different Eye Care Professionals |
| Squint |
| Glaucoma |
| What are floaters? |
| Eye care for children and young adults |
| 兒童護眼常識小冊子 |
| Diabetic retinal diseases |
| Chalazion |
| Care of contact lens |
| Allergic conjunctivitis |
| 親子護眼小冊子 |
| 戰勝黃班病小冊子 |
| 戰勝青光眼小冊子 |
| 青光眼手術 |
| Retinal Detachment |
| Dry Eye Syndrome |
| 白內障 |
| LASER and laser pointers |
| Tear Gas and Pepper Spray |
| Precautions on the use of steroid eyedrops & ointment |
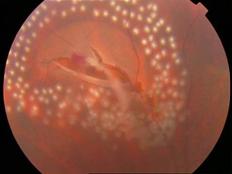
| Retinal Detachment Introduction The retina is a thin, light-sensitive tissue that lines inside the back of the eyeball. Like the film in a camera, the retina converts optical image into nerve impulses that will be transmitted via the optic nerve and perceived as vision in the brain. In most causes retinal detachment is caused by retinal break(s) in the retina which allow fluid to enter beneath the retinal space which results in separation of the retina from the back of the eyeball. Since the detached retina is partially deprived of blood and nutrition supply, it will degenerate and will not function properly. The vision will be impaired and may progress to blindness if left untreated. Different types of retinal detachment There are three different types of retinal detachment: (1) Rhegmatogenous - Retinal detachment is caused by retinal break. The cause is related to age, short-sightedness and the process of vitreous degeneration. This type of retinal detachment is the most common type. (2) Tractional - In this type of detachment, scar tissue on the retina's surface contracts and causes the retina to separate from the RPE due to proliferate vitreoretinopathy or proliferative diabetic retinopathy). (3) Exudative - It is frequently caused by eye diseases including inflammatory disorders and injury/trauma to the eye. In this type of retinal detachment, fluid is secreted into the area underneath the retina, but there is no break in the retina.
Symptoms of retinal detachment Most patients of primary retinal detachment suffer from vision disturbance with no eye redness or pain. It can deteriorate within short period. In the beginning flashing light can be seen, flying dots (floaters), and black shadows seem to move around the visual field. Another symptom is the appearance of a curtain covering part of the visual field. If the detachment involves the macula, the central vision is affected with marked blurred vision and distortion of images. The extent of decrease of vision depends on the location, extent and duration of retinal detachment, and the clarity of vitreous. Who is at risk for retinal detachment? Retinal detachment can occur at any age, but it is more common in people over 40 years of age. It affects men more than women. Retinal detachment is also more likely to occur in people who have:
Treatment Spontaneous resolution of retinal detachment is rare. The usual treatment for retinal detachment is surgery. The procedure includes a combination of cryotherapy, laser therapy, insertion of buckle and / or encircling band, pars plana vitrectomy with injection of gas or silicon oil. The surgical aim is to reattach the retina in order to recover vision. The exact procedure varies with the conditions of patients. Sometimes a patient may need a second or a series of different surgical procedures.
Pre-operative preparation
Post-operative care
Prevention of retinal detachment
Disclaimer: The content of this article is for reference only and does not serve diagnostic or treatment purposes nor does it serve as any recommendation towards the use of particular eye treatment products. | |||||||
© Copyright 2002-2024 The Hong Kong Ophthalmological Society. All rights reserved. |
Phone: (852) 2761 9128 Fax: (852) 2715 0089 Email: info@hkos.org.hk,hkossecretariat@gmail.com |
 Normal Retina Retinal Detachment
Normal Retina Retinal Detachment